Managing with Chronic Pain
Many of us know someone suffering from chronic pain. In Canada, as many as 17% experience some kind of non-specific chronic pain. The cost in lost income, lost productivity and medical expenses are over $10 million a year, yet misconceptions and stigmas overshadow facts.
Defined as any physical discomfort that persists beyond expected healing time, chronic pain can be caused by injuries, failed or unsatisfactory surgeries, and illnesses such as arthritis, osteoporosis, and lupus. Some conditions produce physical changes like joint inflammation or nerve damage, but in others like fibromyalgia there are no clear physical sources for the pain. Lack of clear physical evidence can lead many to question whether the pain is real, but to sufferers it certainly is.
Rates differ among types of chronic pain (e.g., headaches, musculoskeletal, lower back, or joint pain). Regardless, it can be debilitating, limiting people’s abilities to live a full life; leaving many unable to work, engage in social activities and complete basic daily activities. As individuals come to center their world around pain, they withdraw from friends and family, becoming pessimistic about the future and feeling insecure.
Among chronic pain sufferers, the prevalence of depression or anxiety is much higher than in the general population. About 50% of those with chronic pain suffer from some kind of mental illness.
Disorders such as depression and anxiety can be present both before and after pain onset, raising the chicken-egg question of whether mental illness puts you at risk for chronic pain, or whether chronic pain is psychologically damaging.
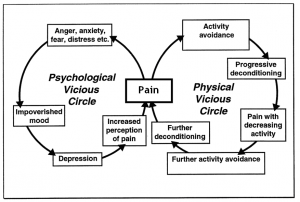
Researchers tend to view the relationship between mental illness and chronic pain as an interaction between biological, psychological and social influences. For those in chronic pain, the brain misinterprets sensations from affected areas. The person is left constantly anticipating pain, leading to stress and anxiety. Increased stress, along with disturbed sleep, social isolation, and depression about one’s life often leaves the sufferer vulnerable to mental illness.
Those who suffer from anxiety or depression often withdraw socially, becoming irritable to those around them. This loss of social support, interaction and activities often exacerbate the symptoms of anxiety or depression, further accentuating pain. A study by psychologist Kati Thieme and colleagues at the University of Washington found that patients with fibromyalgia, an illness that has no identifiable source, who also had an anxiety disorder reported more physical symptoms, impairment in life functioning and the highest levels of pain in comparison to their mentally healthy counterparts.
Since chronic pain often has no clear physical cause, those who suffer from it feel stigmatized, as others may believe the pain is “all in their head.” Health researchers Pia Åsbring and Anna-Liisa Närvänen at Karolinska Institutet and Linköping University respectively, looked at women’s experiences with fibromyalgia, and found that many women reported feeling delegitimized, often accused of “making it up” or having an ulterior motive such as trying to avoid work. Stigma can lead to anxiety, shame and doubt, which can contribute to feelings of worthlessness and hopelessness.
There is no one solution to eliminate chronic pain. Common management strategies are exercise, balanced diet, and good sleep. Over the counter painkillers are also used for pain management and when the pain is more severe, physiotherapy treatment is used to block or desensitize nerves. These treatments help to increase circulation, and recondition muscles that may have been weakened by bed-rest and inactivity.
The relationship between mental illness and chronic pain is complex, so many physicians consider it important to treat the psychological symptoms alongside the physical. They may prescribe psychotropic medication and provide therapy that helps patients develop strategies to cope with the experience of pain.
Acceptance and Commitment Therapy (ACT), a type of behavioural treatment, does just this by teaching patients to accept their thoughts, feelings and physical sensations through mindfulness, helping them cope with symptoms of depression and anxiety. It also uses behaviour change strategies to help them set goals related to different activities of daily living. It is important to resume activities they were able to do before.
The effects of chronic pain are insidious. Stigma and mental illness can make things worse. Without a cure, management strategies are critical so that sufferers don’t let pain take over and ultimately define their lives.
–Jennifer Parlee, Contributing Writer