Is Stanford Neuromodulation Therapy Revolutionizing Treatment of Depression?
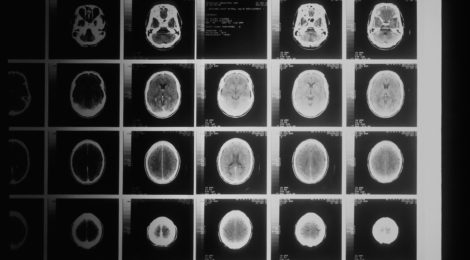
With the development of new neuro-technology and emerging research on the function of the brain, treatment of mental illness has improved immensely to target symptoms at their source. Transcranial Magnetic Stimulation (TMS) was developed in 1985 and considered a breakthrough in treating mental illnesses. TMS works by targeting brain regions associated with mental illness, such as depression, and sends magnetic pulses to excite underactive neurons, helping to improve one’s mood.
In 2020, the Brain Stimulation Lab at Stanford University modified the TMS protocol to increase its effectiveness in treating major depressive disorder. Stanford Neuromodulation Therapy (SNT) works by using functional connectivity magnetic resonance imaging (fcMRI) to target a specific area in the frontal lobes. SNT uses intermittent theta-burst stimulation (iTBS), a form of TMS that delivers magnetic pulses at its own distinct frequency. Putting these methods together allows patients to receive more sessions of treatment per day at lower doses, and complete treatment in just a few days rather than weeks. Research has shown remission rates of close to 90%, making SNT appear to be more effective than many other treatments available.

The Trauma and Mental Health Report (TMHR) interviewed Brandon Bentzley, the co-founder of Magnus Medical, who tells us that SAINT technology is in progress and should be available to the public in 2024. Bentzley also says the global waitlist for SAINT technology is growing rapidly with clinicians and patients interested in the treatment.
Anticipating its release, clinics are beginning to offer SNT treatments without Magnus Medical’s SAINT software. The TMHR interviewed Charles Miller, a nurse anesthesiologist at Scenic City Neurotherapy in Chattanooga, TN, who has been offering Ketamine-infused SNT treatment at his clinic for the past year. Miller tells us his clinic follows SNT protocols strictly, with ten sessions given to the patient for five consecutive days. Ketamine is added to the SNT protocol at the end of days one and five. When comparing Ketamine-Assisted SNT to other treatments offered in clinic, Miller notes higher remission rates and decreases in depressive symptoms. Miller explains it is important to bear in mind that SNT addresses the physiology of depression but does not treat the psychology behind it. This aspect of depression is addressed with the patient’s mental health provider. If the patient does not have a provider, Miller’s clinic refers them to one in the community. “The goal is not to feel better, but to feel the world correctly.”

However, there are reasons to remain somewhat guarded about the effectiveness of SNT.
The The Trauma and Mental Health Report spoke with Khaled Bowarshi from the Florida TMS clinic about the negative aspects of SNT that many fail to mention. Bowarshi agrees that SNT represents an enormous advancement in improving the efficacy of TMS treatment, but mentions that methods used in the SNT protocol were utilized in the past, and this form of treatment is not entirely new.
Bowarshi notes that there is still more research to be done on SNT to demonstrate its effectiveness, highlighting a few critical questions that require investigation. First, is fcMRI the key to SNT’s efficacy, or iTBS? Does the SNT protocol need both methods to be effective, or just one? Also, Bowarshi describes the “fast-on, fast-off” phenomenon, where remission rates have dropped from approximately 80% to 50% one month after finishing treatment. This raises questions around how durable SNT truly is, and underscores the need to have more studies to investigate the long-term effectiveness of the treatment.
Finally, Bowarshi raises skepticism at whether SNT truly is more effective than classic TMS, saying there is room to question whether these treatments are more similar than previously thought. “If something sounds too good to be true, then it probably is.”
The jury may still be out.
-Abigail Ramos, Contributing Writer
Image Credits:
Feature: National Cancer Institute at Unsplash, Creative Commons
First: Sasha Freemind at Unsplash, Creative Commons
Second: K Mitch Hodge at Unsplash, Creative Commons



