
Borderline Personality Disorder Complicates Treatment for Problem Gamblers
Nearly nine of every ten adults in the United States will gamble recreationally at some point in their lives. But for around two percent of adults, gambling will take a darker turn, leading them down a path towards financial, legal, and psychological problems.
According to the fifth edition of the Diagnostic and Statistical Manual for Mental Disorders (DSM-5), individuals must meet four of nine criteria to be diagnosed with a gambling disorder. Problem gambling refers to those who experience harm from gambling, but do not meet full diagnostic criteria for gambling disorder.
Problem gambling is associated with a range of other psychiatric disorders, such as depression, bipolar disorder, anxiety, and substance abuse. Typically, it is treated with various techniques of cognitive behavioral therapy, such as motivational interviewing, identification of triggers and coping strategies, and restructuring of maladaptive thinking patterns.
However, emerging research shows that treatment for gambling problems is often complicated for those also suffering from personality disorders, with borderline personality disorder (BPD) being especially difficult to co-treat.
Debilitating emotional instability is the hallmark of BPD, and symptoms include impulsivity, chronic feelings of emptiness, recurrent threats of self-harm, and a propensity to become involved in intense and unstable interpersonal relationships. These tendencies can severely exacerbate problem gambling.

In 2014, Meredith Brown, Sabura Allen, and Nikki Dowling of Monash University in Australia reviewed existing research to look for patterns linking problem gambling with various personality disorders. They discovered that problem gambling and BPD co-occur frequently in individuals requiring treatment, as opposed to individuals who can control their gambling. Problem gamblers with a diagnosis of BPD are also three times more likely to drop out of treatment.
The reason for this frequent comorbidity may be that similar social and developmental factors contribute to both problem gambling and BPD.
Negative child temperament, impulsivity, and heightened emotional sensitivity characterize both disorders. And both problem gamblers and sufferers of BPD report dysfunctional parent-child interactions, such as a lack of responding to emotional needs, neglect, and sexual abuse.
The researchers also found that core features of BPD—substance abuse, depression, anxiety, and emotion regulation difficulties—are also present in problem gamblers. Problem gamblers and those with BPD also tend to be socially isolated, have problematic relationships with others, are lower on self-esteem, and are more prone to violence.
Brown and colleagues advise that treatment for people with gambling problems should consider screening for BPD. The detection of BPD in problem gamblers can help clinicians plan and customize treatment and improve outcomes. Screening can also prepare clinicians for potential difficulties in treatment and alert them to the need for more stringent behavioural limits during cognitive behavioural therapy.
Screening can also help anticipate the emotional instability central to BPD, which causes patients to act out against clinicians and hospital staff, and contributes to high treatment dropout rates. The tendency of BPD sufferers to see people as “all good” or “all bad” also impacts how they view clinicians who are treating them, which can affect dropout.
These factors add up to individuals with problem gambling and BPD being three times more likely to drop out of treatment than problem gamblers without BPD. Brown explains:
“The fact that problem gamblers have high levels of psychopathology indicates a need to undertake routine and systematic screening and assessment of problem gamblers presenting to treatment facilities. This could be achieved through comprehensive screening for multiple personality disorders or targeted screening of specific personality disorders.”
At the end of their review, Brown and colleagues suggest the use of dialectical behaviour therapy (DBT), which incorporates Eastern philosophies and cognitive behavioural techniques to improve interpersonal effectiveness, emotion regulation, and distress tolerance. Since the approach has been successful in treating aspects of BPD, the researchers suggest that it may also be useful in treating problem gambling and BPD simultaneously.
But the first step is for clinicians to recognize the importance of recognizing those addicted to gambling who also suffer from BPD. Without proper screening, these individuals will continue to be given conventional treatments, which are unlikely to help.
-Veerpal Bambrah, Contributing Writer
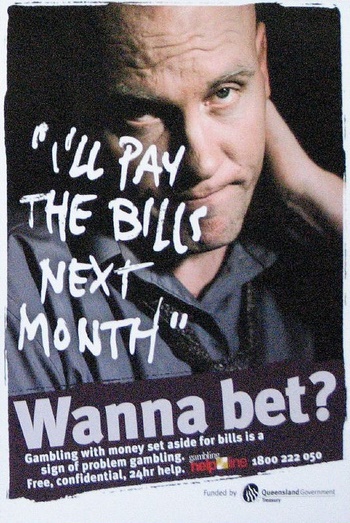
Photo Credits:
Feature: darkHunTer2009 on DeviantArt, Creative Commons
First: Steve Schroeder on Flickr, Creative Commons
Second: Rob and Stephanie Levy on Flickr, Creative Commons



